Stunning
TransformationsTalent and Technology
Love the Way You Look
Our practice balances talent and technology to achieve both quality care and stunning transformations for every client. The rapid advancement of cosmetic, surgical, and medical dermatology can feel overwhelming. That’s why your provider’s dedication to research and individualized patient care play a crucial role in achieving your goals. Taking steps to love the way you look and feel is a valuable investment in your health. At Deschutes Dermatology, our Bend dermatologists are ready to help you on your journey.
DESCHUTES
DERMATOLOGY
BEAUTIFUL,
HEALTHY SKIN
IN CENTRAL OREGON
“My experience at the Deschutes Dermatology center was very pleasing.”
MEDICAL
DERMATOLOGY
Medical Dermatology is dedicated to the diagnosis and treatment of skin, hair, and nail disorders. Treatments may include topical or oral medications, injections, light therapy, and lasers. At Deschutes Dermatology, our experienced Bend dermatologists use the latest, proven methods for treating a wide variety of skin conditions from eczema to psoriasis to rosacea.
SURGICAL
DERMATOLOGY
Surgical Dermatology manages the diagnoses and disorders of the skin and adjacent tissues using various surgical techniques. Surgical procedures are often performed to remove suspicious skin lesions, unwanted moles, and skin cancers of all types. Our Bend dermatologists also commonly remove cysts and growths, revise scars, and repair torn or stretched earlobes with routine, in-office procedures done under local anesthesia.
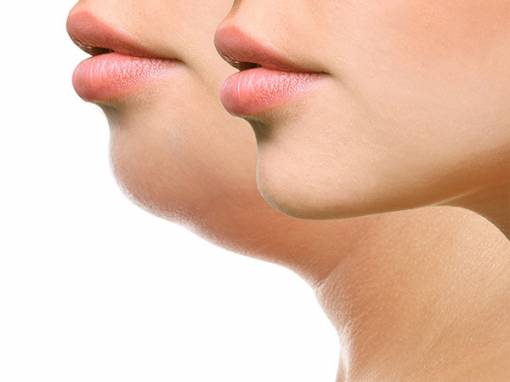
COSMETIC
DERMATOLOGY
Cosmetic Dermatology focuses on the improvement or enhancement in the appearance of your skin for cosmetic and restorative goals. While such treatments are rarely a medical necessity, they can help resolve many skin and aging concerns. Rising in popularity, there were over 15.9 million minimally invasive cosmetic procedures performed in 2016.
MEDICAL
DERMATOLOGY
Medical Dermatology is dedicated to the diagnosis and treatment of skin, hair, and nail disorders. Treatments may include topical or oral medications, injections, light therapy, and lasers. At Deschutes Dermatology, our experienced Bend dermatologists use the latest, proven methods for treating a wide variety of skin conditions from eczema to psoriasis to rosacea.
SURGICAL
DERMATOLOGY
Surgical Dermatology manages the diagnoses and disorders of the skin and adjacent tissues using various surgical techniques. Surgical procedures are often performed to remove suspicious skin lesions, unwanted moles, and skin cancers of all types. Our Bend dermatologists also commonly remove cysts and growths, revise scars, and repair torn or stretched earlobes with routine, in-office procedures done under local anesthesia.
COSMETIC
DERMATOLOGY
Cosmetic Dermatology focuses on the improvement or enhancement in the appearance of your skin for cosmetic and restorative goals. While such treatments are rarely a medical necessity, they can help resolve many skin and aging concerns. Rising in popularity, there were over 15.9 million minimally invasive cosmetic procedures performed in 2016.
“What I find most rewarding about being a Bend dermatologist is the ability to lessen the suffering associated with chronic skin conditions like eczema and psoriasis. It makes such a huge improvement in quality of life when a patient has less rash and itching to deal with. I also love helping patients feel better about their appearance by treating conditions that make them self conscious, like severe acne or wrinkled, sun-damaged skin. I enjoy watching them become more self confident over time as the health of their skin improves.”

Leslie Carter, MD
Dr. Carter